Primary coronary angioplasty during the COVID-19 pandemic
Results from the Stent-Save a Life! international survey on the practice of primary coronary angioplasty during the COVID-19 pandemic.
Authors: Hélder Pereira 1, Christoph Naber 2, Sandrine Wallace 3, Gabor Tóth 4, Sayfollah Abdi 5, Bagrat Alekyan 6, Thomas Alexander 7, Carolina Artucio 8, Ignacio Batista 9, Alfonsina Candiello 10, Rhena Delport 11, Leonardo De Luca 12, Andrejs Erglis 13, Pedro Farto-Abreu 14, Wei-Chung Huang 15, John Kanakakis 16, Michael Lee 17, Awad Mohamed 18, Dejan Orli? 19, Patricio Ortiz 20, Mohamed Sobhy 21, Khaled Shokry 22, Ibrahim Terzic 23, Kyaw Soe Win 24, Jan Piek 25.
The coronavirus (COVID-19) pandemic placed an enormous burden on health services and brought important changes in the social life of populations worldwide (1, 2). Reports have suggested a decrease in the number of patients presenting acute myocardial infarction with an elevation of the ST segment (STEMI) to hospitals (1-12).
STENT-SAVE A LIFE (SSL) aims to improve the delivery of care and patient access to the life-saving indication of primary percutaneous coronary angioplasty (PPCI), thereby reducing mortality and morbidity in patients suffering from acute coronary syndromes (ACS) (13,14). As a global project, SSL member countries from all continents collaborate to develop solutions in order to overcome logistical and organisational barriers preventing today a greater number of patients to have access to the best current treatment for STEMI that is the PPCI. The current pandemic has added new challenges to the difficulties already identified.
The aim of the present analysis was to investigate the reduction rate of PPCI during the COVID-19 outbreak in the beginning of 2020 in countries participating in the SSL global initiative in comparison with the same period in 2019.
Methods
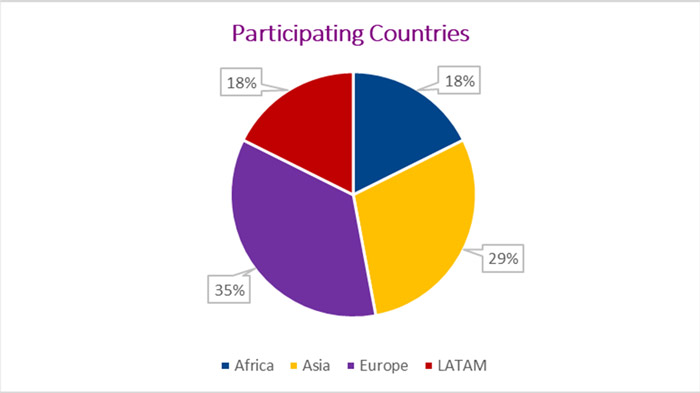
A cross-sectional descriptive and observational study was conducted through a survey in all countries participating in the SSL initiative. From the 32 SSL member countries, 17 accepted to contribute to the survey (3 from Africa, 5 from Asia, 6 from Europe and 3 from Latin America (LATAM)).
The requested data correspond to the period of March and April 2020 in comparison with those from March and April 2019. We collected the data of the number of patients admitted with Acute Coronary Syndromes (ACS), ST elevation myocardial infarction (STEMI) and the numbers of primary PCI (PPCI) conducted
Data sources varied by country; some were national registries, representing the total population whilst others were based on local database collection by the regional SSL group.
Results
Information was received from 17 countries (3 from Africa, 5 from Asia, 6 from Europe and 3 from LATAM).
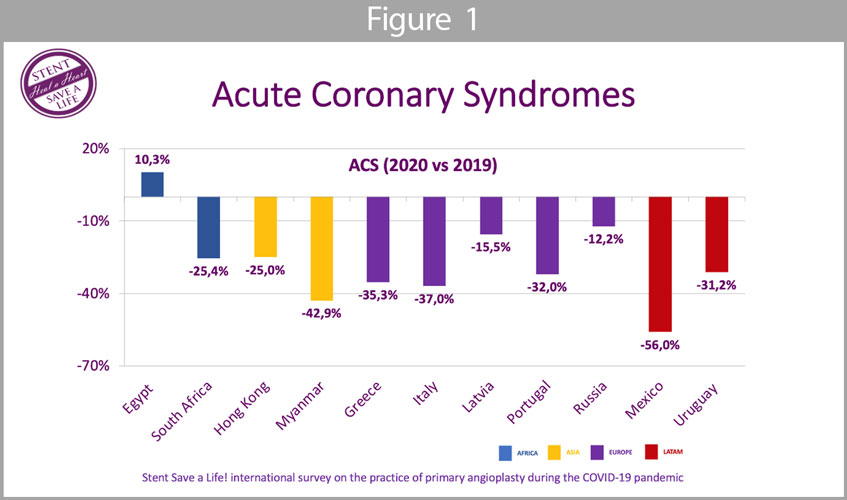
Acute Coronary Syndromes (Figure 1): the mean reduction of ACS patients admitted to the hospital was 27,5%; all countries showed a reduction of admissions with ACS except Egypt where there was an increase of 10,3%. In Myanmar and Mexico, a reduction >40% was observed.
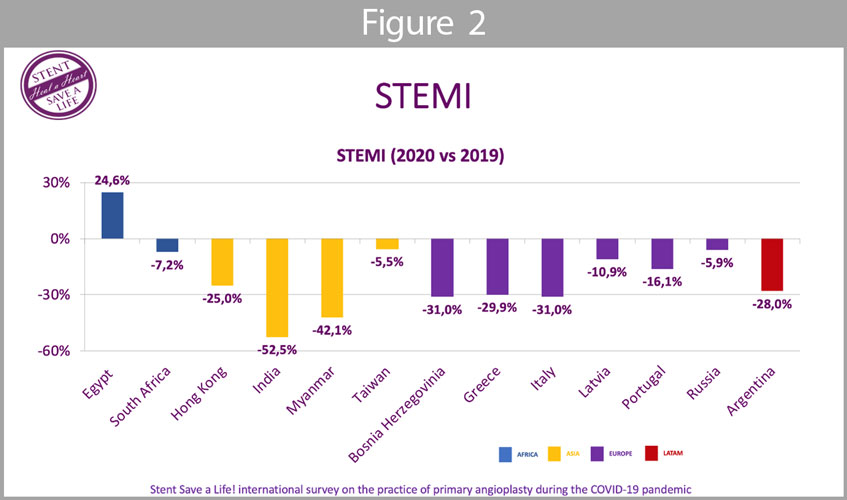
ST-elevation myocardial infarction (Figure 2): the mean reduction of STEMI patients admitted to the hospital was 20,5%; as ACS in general, the particular group of STEMI showed a reduction with the exception of Egypt.
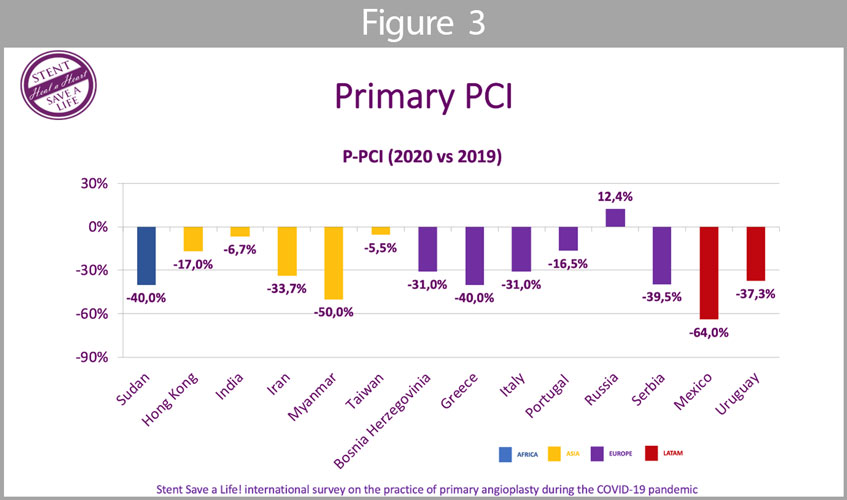
Primary PCI (Figure 3): the mean reduction of PPCI was 26,7%; all countries, except Russia, showed a reduction of PPCI during the pandemic in the 2020 period when compared to the same period in 2019. In Sudan, Myanmar, and Mexico, the reduction was equal or higher than 40%.
Discussion
The results show an important decrease in hospital admissions of patients with ACS and in the numbers of PPCI performed in almost all countries in this survey during the pandemic when compared to the activity in the same period in 2019.
The mean reduction of ACS patients admitted to the hospital was 27,5%, with a reduction of more than 40 % in three countries: Mexico, Myanmar and Sudan. The activity increase observed in Egypt and Russia, according to local SSL officials, are related to the great efforts made in 2019 to expand the capacity for invasive treatment of ACS in those countries, which resulted ultimately in the development of more cath labs and the set-up of STEMI networks. Another explanation is that the period under analysis (March and April 2020) corresponded to the most critical time of the pandemic in Western Europe whereas the peak of incidence in Egypt and Russia occurred later as shown in figure 4 (15).
A report by Mohamed Sobhy (personal communication) from SSL Egypt, revealed that, when the number of patients enrolled in May and June 2019 was compared to the number of patients enrolled in May and June 2020, the number of ACS patients was also reduced. The total number of ACS patients enrolled in the Egyptian registry in May and June 2020 decreased by 18.3%, the number of STEMI cases decreased by 16,0% (16).
Given that the incidence peak outside Western Europe occurred later, these data may lead us to speculate that, in countries where the peak was delayed, the impact would have been even more marked than the one we are reporting for the months of March and April (15).
This reduction in the number of patients admitted to hospitals with STEMI was quickly noticed by the interventional cardiology departments with several centers and societies reporting the phenomenon. In the study by Rodriguez-Leor (3), in Spain, there was a significant decrease in diagnostic procedures (-56%), coronary interventions (-48%), structural interventions (-81%) and in STEMI (-40 %) when comparing homologous periods of 2019 and 2020. Similarly, a reduced rate of hospital admissions for ACS during the COVID-19 outbreak in northern Italy was observed (4). Also in Italy, a nationwide survey collected data on admissions for STEMI throughout a one-week period during the COVID-19 outbreak and observed a 48.4% reduction in admissions for AMI compared with the equivalent week in 2019 (9, 10).
The European Society of Cardiology also launched a worldwide electronic questionnaire that was designed to capture the perception of cardiologists and nurses with regards to the change in frequency and timing of STEMI admissions (17). Overall, there was a perception that the number of admissions of patients with STEMI was substantially reduced by more than 40%.
In other continents, the activity and hospitalisations for ACS were also reduced. A study of 79 centers in 20 countries of Latin America showed a decrease in the number of coronary interventions (–59%) and STEMI care (–51%) (11). In a Taiwanese study, although there was no reduction of the STEMI admissions, a significant delay for medical help was found during the COVID-19 pandemic (12). While the incidence in the United States started later than in Europe, a study from two North American centres also observed a 9.5% reduction in patients diagnosed with STEMI in March 2020 when compared to March 2019 (5). Another study, based on data from 21 medical centres in Northern California, showed that the weekly rates of hospitalisation for acute myocardial infarction decreased by up to 48% during the COVID-19 period, when the authors compared the first reported death from COVID-19 on March 4, 2020 with the same period in 2019 (6). Garcia (7) also observed a 38% reduction in US cardiac catheterisation laboratory STEMI activation. A study by Tam (8) from Hong Kong, China, drew attention to the impact of Coronavirus Disease 2019 in time components of STEMI patients. The patient delay was 318 min during the epidemic period and 83 min in previous period (8).
Information on the increase of “patient delay” and “system delay” is still scarce but, given that a large saturation of the health systems has been observed, particularly in terms of emergencies and intensive care, it leads us to speculate that STEMI patients could have been impacted in terms of timely access to primary angioplasty.
The causes for the reduction in the number of PPCI are probably multifactorial and we can only speculate. What is known is that the number of patients admitted to hospitals and treated by PPCI was reduced. The most obvious explanation is that patients avoided hospitals for fear of becoming infected, but we also have no data to refute the possibility of a real reduction in the incidence of acute coronary syndromes. Based on the Lombardia Cardiac Arrest Registry, Baldi (17) compared out-of-hospital cardiac arrests (OHCA) during the pandemic period in Italy with the same period in 2019 and observed an increase of 58% of OHCA, which supports the hypothesis that ACS patients chose not to go to the hospital.
The Stent-Save a Life (13, 14) global initiative has the mission to reduce mortality from acute myocardial infarction. The so-called “patient delay”, i.e. the time gap from symptom onset until patients seek medical attention, is multifactorial but results largely from a failure to correctly identify the symptoms of a potential ACS and, in countries with less resources or without organised networks, in the difficulties for patients to reach the health services (18, 19). At a time when we are facing a highly contagious epidemic, while flooded with televised images of disrupted hospitals and permanently warned to stay at home by the authorities, the natural reaction is to lessen the symptoms and avoid visiting an hospital.
Finally, it is also unclear whether a true reduction in the number of acute coronary syndromes was observed at the same time. The drop in physical exercise due to lockdown, the adoption of teleworking, the reduction of the atmospheric pollution and other related drastic changes in our habits may have had an effect on the stability of atherosclerotic plaques (20).
It was soon realised that patients with COVID-19 had significant secondary cardiovascular disorders and complications; moreover, patients with a cardiovascular history were more likely to develop unfavorably (21-22). Several scientific societies have commented on the management of both cardiovascular patients with COVID-19 (22-24) and angiography rooms (26-28).
Scientific societies are advocating the deferral of elective procedures. This implies that, during this period, the populations no longer have access to important advances observed in the last decades as far as the diagnosis and treatment of cardiovascular diseases.
We still don’t know how long this pandemic will last and how many months or years we will have to work in a protected environment. All the logistics to deal with the COVID-19 issues, even outside infection peaks, require an enormous enhancement of material and human capabilities.
Many of the SSL member countries were already struggling with a great scarcity of resources that is now exacerbated due to the COVID-19. Governments and hospital administrations themselves, when trying to respond to the public opinion, may tend to focus more on the COVID-19 crisis neglecting cardiovascular diseases in some way.
It is up to the cardiology societies, in general, and the SSL global initiative in particular, to advocate the need for ACS patients to maintain the quality care that this pathology deserves.
Limitations
The main limitation is that it is a retrospective study that doesn’t represent all the countries that are members of the Stent-Save a Life global initiative. Another limitation lies in the fact that neither the “patient delay” nor the “system delay” times were obtained and that no data on mortality was provided. In a period of such great burdens for hospitals, it would have been very difficult for the teams to obtain further prospective data than those that have been requested.
Conclusions
In conclusion, in addition to the COVID-19 direct effects on the cardiovascular system, this pandemic could also contribute to increase the mortality by reducing the admissions of patients to hospitals.
It is important that countries involved in the SSL global initiative raise the alert for patients with ACS in general, and STEMI in particular, developing awareness campaigns for populations to recognise symptoms and not waste time. Simultaneously, it is important that adequate efforts are made so that hospital organisations, when focused on treating COVID patients, do not neglect other patient cohorts including those with acute coronary syndromes.
It is also important to ensure that the diagnostic and therapeutic activity is gradually resumed in safe conditions for both patients and professionals.
Impact on daily practice
This survey clearly demonstrated a reduction, globally, in patients hospitalised with acute coronary syndromes and primary angioplasty procedures. Meanwhile, cardiovascular diseases continue to manifest themselves and consequently it is necessary to warn decision-makers to not forget this pathology and establish action plans and protocols that aim to overcome the barriers imposed by the pandemic crisis.
1 SSL Europe, Hospital Garcia Orta, Almada, Portugal and Lisbon School of Medicine of the University Lisbon, Portugal, 2 SSL Chairman, Klinikum Wilhelmshaven GmbH, Wilhelmshaven, Germany, 3 SSL Global Project Manager, 4 SSL Europe, University Heart Center Graz, Medical University of Graz, Austria, 5 SSL Iran, Rajaie Cardiovascular Medical and Research Center, Iran University of Medical Sciences, Tehran, Iran, 6 SSL Russia, Academician of the Russian Academy of Science, A.V. Vishnevsky Institute of Surgery, Moscow, 7 SSL India, Kovai Medical Centre and Hospital, Coimbatore, India, 8 SSL Uruguay, Instituto de Cardiología Intervencionista de Casa de Galicia, Montevideo; Uruguay, 9 SSL Uruguay, Centro Cardiológico Americano, Montevideo, Uruguay, Hemodinamia del Litoral, Salto, Uruguay, 10 SSL Argentina, Instituto Cardiovascular de Buenos Aires, Buenos Aires, Argentina, 11 SSL South Africa, Department of Family Medicine, Steve Bico Academic Hospital, School of Medicine, Faculty of Health Sciences, University of Pretoria, South Africa, 12 SSL Italy, Dept of Cardiosciences, Azienda Ospedaliera San Camillo-Forlanini, Rome, Italy, 13 SSL Latvia, University of Latvia, Pauls Stradins Clinical University Hospital, Riga, Latvia, 14 SSL Portugal, Cardiology Department, Amadora, Portugal, 15 SSL Taiwan, Department of Critical Care Medicine, Kaohsiung Veterans General Hospital and Department of Physical Therapy, Fooyin University, Kaohsiung, and School of Medicine, National Yang-Ming University, Taipei, Taiwan, 16 SSL Greece, Department of Clinical Therapeutics, University of Athens, Alexandra Hospital, Athens, Greece, 17 SSL Asia, Division of Cardiology, Department of Medicine, Queen Elizabeth Hospital, Hong Kong SAR, China, 18 SSL Sudan, University of Khartoum, Sudan, 19 SSL Serbia, Cardiology Clinic, Clinical Centre of Serbia, Faculty of Medicine, University of Belgrade, Serbia, 20 SSL Mexico, Instituto Nacional de Cardiología “Ignacio Chávez”, Cardiosur, Instituto Cardiovascular Cuernavaca, Medica Sur, Mexico, 21 SSL Egypt; Faculty of Medicine, Alexandria University, Alexandria, Egypt, 22 SSL Egypt, Dean of Military Faculty of Medicine, Cairo, Egypt, 23 SSL Bosnia and Herzegovina, President of WG of Interventional Cardiology, Bosnia and Herzegovina, Cardiocenter Terzic, Tuzla, Bosnia and Herzegovina, 24 SSL Myanmar, Upper Myanmar Heart Centre, Mandalay, Myanmar, 25 SSL Co-chairman, Academisch Medisch Centrum Universiteit van Amsterdam – AMC Heart Center, Amsterdam, Holland
Bibliography
(1) Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X , Guan L, Wei Y, Li H, Xudong X, Xu J, Tu S, Zhang Y, Chen H, Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020;395(10229):1054-62. DOI:https://doi.org/10.1016/S0140-6736(20)30566-3
(2) Grasselli G, Pesenti A, Cecconi M. Critical Care utilization for the COVID-19 outbreak in Lombardy, Italy: early experience and forecast during an emergency response. JAMA 2020;323:1545-6. doi:10.1001/jama.2020.4031
(3) Rodríguez-Leor O, Cid-Álvarez B, Ojeda S, Martín-Moreiras J, Rumoroso J, López-Palop R , Serrador A, Cequier A, Romaguera R, Cruz I, Armando Pérez de Prado, Moreno R. Impact of the COVID-19 pandemic on healthcare activity in interventional cardiology in Spain. REC Interv Cardiol. 2020; https://doi.org/10.24875/RECIC.M20000120
(4) De Filippo O, D’Ascenzo F, Angelini F, Bocchin P, Conrotto, F Saglietto A. Reduced rate of hospital admissions for ACS during Covid-19 outbreak in northern Italy. N Engl J Med. DOI:10.1056/NEJMc2009166.
(5) Zitelny E, Newman N, Zhao D. STEMI during the COVID-19 Pandemic – An Evaluation of Incidence, Cardiovascular Pathology (2020), doi: https://doi.org/10.1016/j.carpath.2020.107232
(6) Solomon M, McNulty E, Rana J, Leong T, Ambrosy A, Sidney S. The Covid-19 pandemic and the incidence of acute myocardial infarction. N Engl J Med. DOI: 10.1056/NEJMc2015630.
(7) Garcia S, Albaghdadi M, Meraj P, Schmidt C, Garberich R, Jaffer F, Dixon S, Rade J, Tannenbaum M, Chambers J, Huang P, Henry T. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the united states during COVID-19 pandemic, Journal of the American College of Cardiology (2020), doi: https://doi.org/10.1016/j.jacc.2020.04.011.
(8) Tam CF, Cheung KS, Lam S, Wong A, Yung A, Sze M, Lam, YM, Chan C, Tsang TC, Tsui M, Tse HF, Siu CW. Impact of coronarvirus disease 2019 (COVID-19) outbreak on ST-segment elevation myocardial infarction care in Hong-Kong, China. Circ Cardiovasc Qual Outcomes. 2020. https://doi.org/ 10.1161/CIRCOUTCOMES.120.006631.
(9) Metzler B, Siostrzonek P, Binder R, Bauer A, Reinstadler S. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID-19: the pandemic response causes cardiac collateral damage. Eur Heart J 2020;41:1852-3. doi: 10.1093/eurheartj/ehaa314
(10) De Rosa S, Spaccarotella C, Basso C, Calabrò M, Curcio A, Filardi P, Mancone M, Mercuro G, Muscoli S, Nodari S, Pedrinelli R, Sinagra G, Indolfi C. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur Heart J 2020 ehaa409. https://doi.org/10.1093/eurheartj/ehaa409
(11) Mayol J, Artucio C, Batista I, Puentes A, Villegas J, Quizpe R, Rojas V, Mangione J, Belardi J J. An international survey in Latin America on the practice of interventional cardiology during the COVID-19 pandemic, with a particular focus on myocardial infarction. Neth Heart J. 2020; 28:424-430. doi 10.1007/s12471-020-01440-y
(12) Li YH, Huang WC, Hwang JJ; Taiwan Society of Cardiology. No Reduction of ST-segment elevation myocardial infarction admission in taiwan during coronavirus pandemic. Am J Cardiol. 2020 Jun 27:S0002-9149(20)30607-X. doi: 10.1016/j.amjcard.2020.06.030
(13) Widimsky P, Fajadet J, Danchin N, Wijns W. “Stent 4 Life” targeting PCI at all who will benefit the most: A joint project between EAPCI, Euro-PCR, EUCOMED and the ESC working group on acute cardiac care. EuroIntervention. 2009;4(5):555-557. doi:10.4244/EIJV4I5A94
(14) https://www.stentsavealife.com/ (assessed date: 24th May 2020)
(15) https://ourworldindata.org/coronavirus/country/india?country=~IND (assessed date 26th July 2020)
(16) Pessoa-Amorim G, Camm C, Gajendragadkar P, De Maria G, Arsac C, Laroche C, Zamorano J, Weidinger F, Achenbach S, Maggioni A, Gale C, Poppas A, Casadei B. Admission of patients with STEMI since the outbreak of the COVID-19 pandemic. A survey by the European Society of Cardiology Heart Journal – Quality of Care and Clinical Outcomes, qcaa046, https://doi.org/10.1093/ehjqcco/qcaa046
(17) Baldi E, Sechi G, Primi R, Mare C, Canevari F, Brancaglione A, Primi R, Klersy C, Palo A, Contri E, Ronchi V, Beretta G, Reali F, Parogni P, Facchin F, Bua D, Rizzi U, Bussi D, Ruggeri S, Visconti L, Savastano S. Out-of-hospital cardiac arrest during the Covid-19 outbreak in Italy. N Engl J Med 2020; 383:496-498 DOI: 10.1056/NEJMc2010418
(18) Pereira H, Calé R, Pinto F, Pereira E, Caldeira D, Mello S, Vitorino S, Almeida M, Mimoso J. Factors influencing the patient delay to primary angioplasty in myocardial infarction with ST-segment elevation. Rev Port Cardiol. 2018;37:409-421. doi: 10.1016/j.repc.2017.07.014.
(19) Pereira H, Pinto F Calé R, Pereira E, Mello S, Vitorino S, Sousa P, Brochado B, Monteiro S, Teles R. Stent for Life initiative: predictive factors of system delay in patients with ST-segment elevation myocardium infarction (STEMI). Rev Port Cardiol. 2018;37:681-690. doi: 10.1016/j.repc.2018.01.011
(20). Kato A, Minami Y, Katsura A, Muramatsu Y, Sato T, Kakizaki R, Nemoto T, Hashimoto T, Fujiyoshi K, Meguro K, Shimohama T, Ako J. Physical exertion as a trigger of acute coronary syndrome caused by plaque erosion. J Thromb 221 Thrombolysis 2020;49:377—85. DOI: 10.1007/s11239-020-02074-y
(21) Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus—infected pneumonia in Wuhan, China. JAMA 2020;323:1061–9. doi:10.1001/jama.2020.1585
(22) Driggin E, Madhavan M, Bikdeli B, Chuich T, Laracy J, Biondi-Zoccai G, Brown T, Nigoghossian C,. Zidar D, Haythe J, Brodie D, Beckman J, Kirtane A, Stone G, Krumhol H, Parikh S. Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic. J Am Coll Cardiol;75:2352-71 2020 DOI: 10.1016/j.jacc.2020.03.031
(23) ESC Guidance for the Diagnosis and Management of CV Disease during the COVID-19 Pandemic. https://www.escardio.org/Education/COVID-19-and-Cardiology/ESC-COVID-19-Guidance (assessed date: 24th May 2020)
(24) Mahmud E, Dauerman HL, Welt FG, Messenger J, Rao S, Grines C, Mattu A, Kirtane A, Jauhar R, Meraj P, Rokos I, Rumsfeld J, Henry T. Management of acute myocardial infarction during the COVID-19 pandemic, Journal of the American College of Cardiology (2020), doi: https://doi.org/10.1016/j.jacc.2020.04.039.
(25) Kerkar P, Naik N, Alexander T, Bahl V, Chakraborty R, Chatterjee S, Chopra H, Dani S, Deb P, Goswami K, Guha S, Gupta R, Gupta V, Hasija P, Jayagopal P, Justin Paul G, Kahali D, Katyal V, Khanna N, Mandal M, Mishra S, Mohanan P, Mullasari A, Mehta S, Pancholia A, Ray S, Roy D, Shanmugasundarm S, Sharma S, Singh B, Tewari S, Tyagi S, Venugopal K, Wander G, Yadav R, Das M. Cardiological Society of India: Document on acute MI care during COVID-19, Indian Heart Journal, https://doi.org/10.1016/j.ihj.2020.04.009.
(26) Welt F, Shah P, Aronow H, Bortnick A, Bortnick A, Henry T, Sherwood M, Young M, Davidson L, Kadavath S, Mahmud E, Kirtane A. Catheterization laboratory considerations during the coronavirus (COVID-19) pandemic: From ACC’s Interventional Council and SCAI. JACC 2020. http://dx.doi.org/10.1016/j.jacc.2020.03.021.
(27) Romaguera R, Cruz-Gonzalez I, Ojeda S, Jiménez-Candil J, Calvo D, eara J, Cañadas-Godoy V, Calvo E, Brugaletta S, Ledesma M, Moreno R. Consensus document of the Interventional Cardiology and Heart Rhythm Associations of the Spanish Society of Cardiology on the management of invasive cardiac procedure rooms during the COVID-19 coronavirus outbreak. REC Interv Cardiol 2020. http://dx.doi.org/10.24875/RECICE.M20000116) (Article in press, available online)
(28) Lo S, Yong A, Sinhal A, Shetty S, McCann A, Clark D, Galligan L, El-Jack S, Sader M, Tan R, Hallani H, Barlis P, Sechi R, Dictado E, Walton A, Starmer G, Bhagwandeen R, Leung D, Juergens C, Bhindi R, Muller D, Rajaratnum R, French J, Kritharides L. Consensus Guidelines for Interventional Cardiology Services Delivery During COVID-19 Pandemic in Australia and New Zealand. Heart, Lung and Circulation (2020), https://doi.org/10.1016/j. hlc.2020.04.002